In order to bridge the gap between clinical outcome and the underlying predictive molecular and physiological mechanisms, medicine relies on precise and powerful indicators called biomarkers. These measurable molecules or biological characteristics allow for earlier diagnosis, more accurate monitoring of disease progression and responsiveness to the therapeutic interventions thus providing the basis for personalised treatment strategies. Despite their transformative impact on diagnostics, prognostics and drug development, challenges remain regarding their specificity, sensitivity, and standardisation across different settings. How can we fully discover the potential of biomarkers and revolutionise patient care? We’ll find out in this article, along with the unique use of biomarkers in the Neuromind device.
Biomarkers decoded: Unraveling nature's signals
A biomarker, short for biological marker, is any measurable biological parameter that can be used to assess health or disease states. According to the U.S. National Institutes of Health (NIH), a biomarker is defined as: “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention.” [1]
Simply put, biomarkers are like signposts that provide clues about what’s happening inside our bodies.
A biological marker can refer to any measurable indicator derived from biological processes. For example, biomarkers may be observed at both cellular and molecular levels (including DNA, RNA, proteins and metabolites).
Biomarkers are obtained from either tissue samples or liquid biopsies (blood, urine, saliva, etc.). Additionally, other types of biomarkers—such as those reflecting physiological or morphological characteristics—can be captured using clinical or medical imaging techniques such as electroencephalography (EEG) or functional magnetic resonance imaging (fMRI).
Biomarkers can be categorized as either quantitative or qualitative:
– qualitative biomarkers are generally used in binary analyses to determine the presence or absence of a pathological process;
– quantitative biomarkers help identify a disease process once a specific threshold is exceeded.

Classification of biomarkers: The spectrum of signaling
Biomarkers can be classified based on their applications and the information they provide. [2][3][4]
Diagnostic biomarkers
The diagnostic biomarkers help in the identification of a disease or condition at an early stage. For instance, elevated levels of prostate-specific antigen (PSA) can serve as an early indicator of prostate cancer.
Prognostic biomarkers
Prognostic biomarkers provide information about the likely course or outcome of a disease. For example, certain gene expression profiles in tumors can predict the aggressiveness of cancer and guide treatment decisions.
Predictive biomarkers
Predictive biomarkers are used to identify the likelihood of a patient’s response to a specific treatment. For example, the presence of the HER2 protein in breast cancer cells predicts a better response to trastuzumab, a targeted therapy.
Pharmacodynamic biomarkers
Pharmacodynamic biomarkers indicate the biological response to a therapeutic intervention in real time. For example, the Bispectral Index (BIS), a derived EEG parameter, is used to monitor the level of consciousness during surgery.
Surrogate endpoints
In clinical research, surrogate endpoints are biomarkers intended to substitute for a clinical endpoint. They can provide earlier insights into treatment effects and are particularly useful when the true clinical endpoints require long-term observation.
Examples of biomarkers in medicine
The practical applications of biomarkers in medicine are vast. Here are a few prominent examples.
1. Cardiac biomarkers
Troponin: Elevated levels of cardiac troponin in the blood are a well-established indicator of myocardial infarction (heart attack). Troponin levels rise when heart muscle is damaged, making it a critical diagnostic marker in emergency care. [5]
B-type Natriuretic Peptide (BNP): BNP is used to assess heart failure. Higher levels of BNP can indicate that the heart is struggling to pump blood efficiently. [6]
2. Oncological biomarkers
Prostate-Specific Antigen (PSA): PSA is a protein produced by the prostate gland, and its elevated levels are used to screen for prostate cancer. Despite some controversy regarding its specificity, PSA remains a widely used biomarker. [7][8]
BRCA1/BRCA2 Genes: Mutations in these genes significantly increase the risk of breast and ovarian cancers. Testing for these mutations can guide preventive strategies and personalised treatment plans. [9][10]
Carcinoembryonic Antigen (CEA): This protein is often elevated in individuals with colorectal cancer and is used to monitor treatment response and recurrence. [11]
3. Inflammatory biomarkers
C-reactive Protein (CRP): CRP is produced by the liver in response to inflammation. High levels of CRP are associated with various conditions, including infections, autoimmune diseases, and cardiovascular diseases. [12]
Erythrocyte Sedimentation Rate (ESR): Although less specific than CRP, ESR is a common biomarker used to assess the presence and intensity of inflammation in the body. [13]
4. Neurological biomarkers
Beta-amyloid and Tau Proteins: In Alzheimer’s disease, abnormal accumulation of beta-amyloid plaques and tau protein tangles in the brain is a hallmark of the pathology. Measuring these proteins in cerebrospinal fluid (CSF) or through imaging techniques can aid in early diagnosis. [14][15][16]

Applications of biomarkers in research and personalised medicine
The utility of biomarkers extends far beyond diagnosis. In drug development, biomarkers are used to:
– enhance clinical trial design: by identifying patients who are most likely to respond to a new therapy, biomarkers can help stratify patient populations and improve the efficiency of clinical trials;
– monitor drug efficacy and safety: biomarkers provide a means to monitor the biological effects of a drug, thereby offering early indications of efficacy and potential side effects;
– guide personalised treatment: in the era of personalised medicine, biomarkers enable healthcare providers to tailor treatments to the genetic and molecular profiles of individual patients, improving outcomes and minimising adverse effects.
In research settings, biomarkers are essential for understanding disease mechanisms. They offer insights into the molecular pathways that drive disease progression and help identify potential therapeutic targets.
For example, the identification of specific genetic biomarkers in cancer has led to the development of targeted therapies that inhibit key molecular pathways involved in tumor growth.
Challenges in biomarker development
Despite their potential, the development and implementation of biomarkers face several challenges. [4]
Specificity and sensitivity
A biomarker must be both highly specific to a particular disease and sensitive enough to detect early or subtle changes. However, many biomarkers can be influenced by multiple factors, which can compromise their diagnostic accuracy.
Standardisation
Variability in sample collection, processing, and analysis can lead to inconsistent results. Developing standardised protocols is key for ensuring that biomarker measurements are reliable and reproducible across different laboratories and clinical settings.
Regulatory hurdles
Before being adopted in clinical practice, biomarkers must undergo rigorous validation and regulatory approval. This process can be time-consuming and expensive, potentially delaying the transition of promising biomarkers from research to clinical use.
Biological complexity
Diseases often involve complex interactions among various biological pathways. A single biomarker may not capture the full picture of a disease process. Therefore, using biomarker panels or a combination of markers is sometimes necessary to achieve accurate diagnosis and prognosis.

Neuromind: A unique device combining proprietary attention & emotion biomarkers
Neuromind is an innovative neurofeedback solution that combines advanced sensor technologies with immersive virtual reality to measure and modulate emotional states.
Developed by a research team combining experts in neuroscience and data science, in collaboration with a scientific committee of the renowned experts, our device emerged from a psychophysiological study at the Paris Brain Institute. We collected electrophysiological data from both the central and peripheral nervous systems to identify new emotional biomarkers.
Using machine learning algorithms, Neuromind translates brain activity into two key emotional parameters:
– arousal (reflecting energy or calmness);
– valence (indicating the positivity or negativity of an emotion).
These biomarkers allow the system to map a user’s emotional state in real time, creating a clear picture of their current mood. This information is then used in a closed-loop system where the virtual reality environment adapts dynamically to guide the user toward a desired state, such as relaxation or mindfulness.
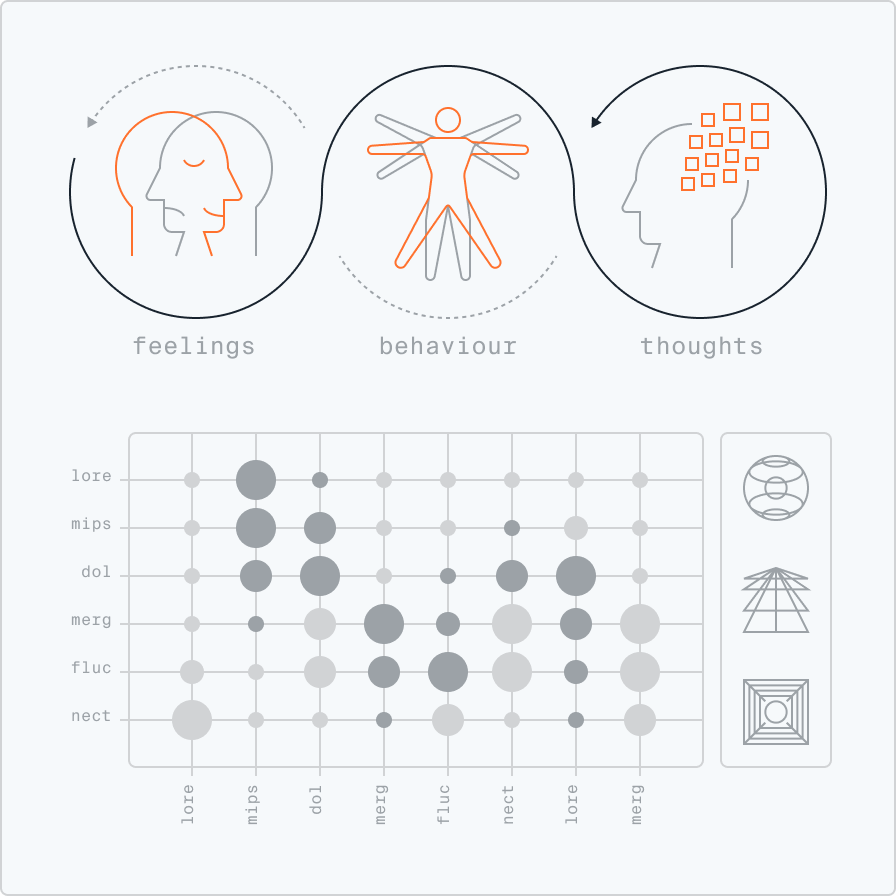
This adaptive immersion not only supports therapeutic interventions for conditions like depression but also provides a valuable tool for research and treatment optimisation. Recognised for its potential, Neuromind has garnered awards and industry support, marking a significant step forward in the field of digital health and neuroscience.
Looking ahead, biomarkers will continue to play an essential role in the advancement of personalised medicine. Their ability to provide real-time insights holds promise for more targeted and effective therapies. Innovative devices such as Neuromind are already pushing these boundaries by integrating electrophysiological monitoring with adaptive virtual reality to fine-tune emotional states and enhance therapeutic outcomes. This cutting-edge solution not only exemplifies the practical application of biomarkers but also paves the way for improved patient care in mental health and beyond. If you’d like to find out how our device works, we’d be delighted to arrange a demonstration.
[1] Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69:89-95.
[2] U.S. Department of Health and Human Services. Biomarkers Toolkit.
[3] Baker SG, Kramer BS. Simple Methods for Evaluating 4 Types of Biomarkers: Surrogate Endpoint, Prognostic, Predictive, and Cancer Screening. Biomark Insights. 2020 Aug 4;15:1177271920946715. doi: 10.1177/1177271920946715. PMID: 32821082; PMCID: PMC7412628.
[4] Califf RM. Biomarker definitions and their applications. Exp Biol Med (Maywood). 2018 Feb;243(3):213-221. doi: 10.1177/1535370217750088. PMID: 29405771; PMCID: PMC5813875.
[5] Apple FS, Sandoval Y, Jaffe AS, Ordonez-Llanos J; IFCC Task Force on Clinical Applications of Cardiac Bio-Markers. Cardiac Troponin Assays: Guide to Understanding Analytical Characteristics and Their Impact on Clinical Care. Clin Chem. 2017 Jan;63(1):73-81. doi: 10.1373/clinchem.2016.255109. Epub 2016 Oct 10. PMID: 28062612.
[6] Vuolteenaho O, Ala-Kopsala M, Ruskoaho H. BNP as a biomarker in heart disease. Adv Clin Chem. 2005;40:1-36. PMID: 16355919.
[7] David MK, Leslie SW. Prostate-Specific Antigen. [Updated 2024 Sep 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557495/
[8] Henry NL, Hayes DF. Cancer biomarkers. Mol Oncol. 2012 Apr;6(2):140-6. doi: 10.1016/j.molonc.2012.01.010. Epub 2012 Feb 6. PMID: 22356776; PMCID: PMC5528374.
[9] Miki Y, Swensen J, Shattuck-Eidens D, Futreal PA, Harshman K, Tavtigian S, Liu Q, Cochran C, Bennett LM, Ding W, et al. A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science. 1994 Oct 7;266(5182):66-71. doi: 10.1126/science.7545954. PMID: 7545954.
[10] Wooster R, Bignell G, Lancaster J, Swift S, Seal S, Mangion J, Collins N, Gregory S, Gumbs C, Micklem G. Identification of the breast cancer susceptibility gene BRCA2. Nature. 1995 Dec 21-28;378(6559):789-92. doi: 10.1038/378789a0. Erratum in: Nature 1996 Feb 22;379(6567):749. PMID: 8524414.
[11] Duffy MJ. Carcinoembryonic antigen as a marker for colorectal cancer: is it clinically useful? Clin Chem. 2001 Apr;47(4):624-30. PMID: 11274010.
[12] Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003 Jun;111(12):1805-12. doi: 10.1172/JCI18921. Erratum in: J Clin Invest. 2003 Jul;112(2):299. PMID: 12813013; PMCID: PMC161431.
[13] Saadeh C. The erythrocyte sedimentation rate: old and new clinical applications. South Med J. 1998 Mar;91(3):220-5. PMID: 9521358.
[14] Jack CR Jr, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, Petersen RC, Trojanowski JQ. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010 Jan;9(1):119-28. doi: 10.1016/S1474-4422(09)70299-6. PMID: 20083042; PMCID: PMC2819840.
[15] Blennow K, de Leon MJ, Zetterberg H. Alzheimer’s disease. Lancet. 2006 Jul 29;368(9533):387-403. doi: 10.1016/S0140-6736(06)69113-7. PMID: 16876668.
[16] Sharma VK, Singh TG, Mehta V, Mannan A. Biomarkers: Role and Scope in Neurological Disorders. Neurochem Res. 2023 Jul;48(7):2029-2058. doi: 10.1007/s11064-023-03873-4. Epub 2023 Feb 16. PMID: 36795184.
